Repeated Administration of 2-Hydroxypropyl-β-Cyclodextrin (HPβCD) Attenuates the Chronic Inflammatory Response to Experimental Stroke
Full title: Repeated Administration of 2-Hydroxypropyl-β-Cyclodextrin (HPβCD) Attenuates the Chronic Inflammatory Response to Experimental Stroke
Publication authors: Danielle A. Becktel, Jacob C. Zbesko, Jennifer B. Frye, Amanda G. Chung, Megan Hayes, Kylie Calderon, Jeffrey W. Grover, Anna Li, Frankie G. Garcia, Marco A. Tavera-Garcia, Rick G. Schnellmann, Hsin-Jung Joyce Wu, Thuy-Vi V. Nguyen and Kristian P. Doyle
Summary author: Momina Atique
Full publication link: https://doi.org/10.1523/JNEUROSCI.0933-21.2021 [doi.org]
Key Words
Ischemic stroke – the most common type of stroke, occurs when a blood vessel supplying the brain becomes blocked.
Cognitive decline – occurs as a consequence of stroke when an individual’s mental ability is affected, including problems with memory, communication, concentration and decision-making.
Immune system – our body’s natural defence mechanism against infection and injury, helps to initiate repair of any damage.
Chronic inflammatory response – when our immune response continues for a long period of time, even in the absence of any injury. If it becomes uncontrolled, it can lead to more damage.
Lipids – fatty substances found in all cells of the body, involved in a variety of different functions
2-Hydroxypropyl-β-cyclodextrin (HPβCD) – a compound which reduces build up of lipids, stimulating an anti-inflammatory response. Investigated in this study as a potential treatment for cognitive decline after stroke.
What is an ischemic stroke and how is the immune system involved?
- An ischemic stroke is caused by the blockage of a blood vessel in the brain, meaning the cells in the brain cannot get enough oxygen and nutrients and will eventually die.
- Globally, it is a leading cause of death and disability.
- ⅓ of survivors slowly develop cognitive decline, which includes problems with communication, language, movement and memory.
- Whilst the immune system is initially activated after a stroke to repair the damaged brain, stroke survivors develop a prolonged and uncontrolled immune response, making repair and recovery more difficult.
- Currently, scientists are trying to understand how this chronic inflammatory response could lead to cognitive decline, in the hopes of developing treatments to improve outcomes of stroke patients.
Background of this study
- During a stroke, cells in the brain burst and die, causing different molecules to be released that may trigger an immune response.
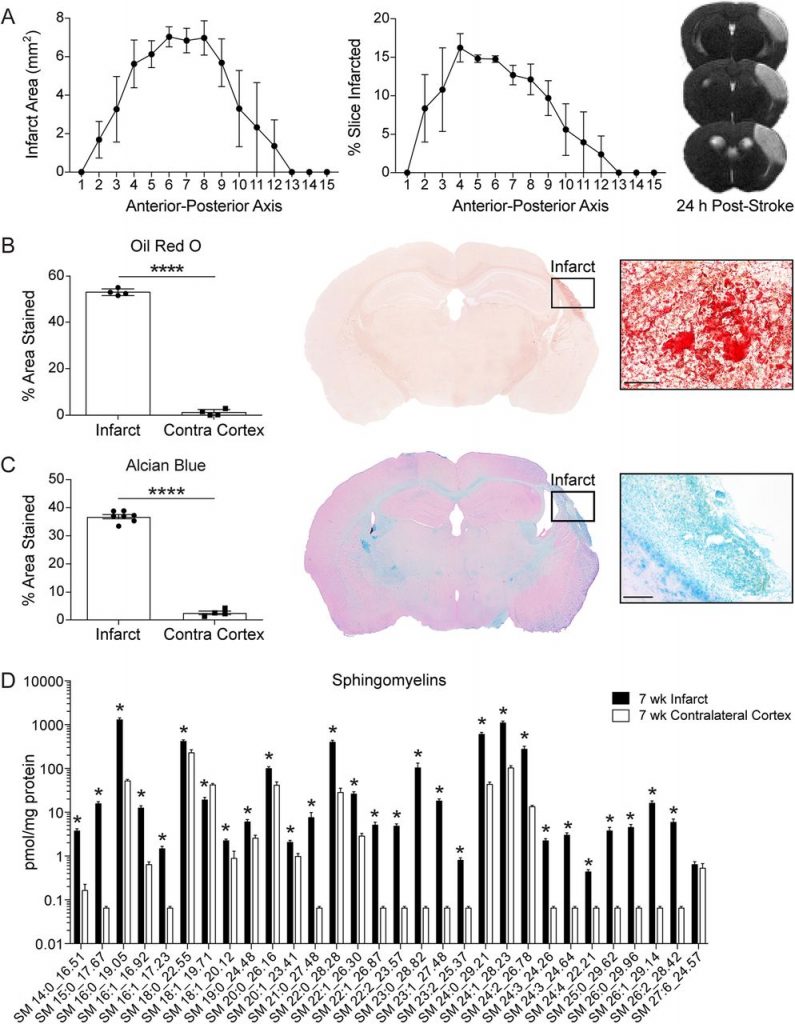
- This study wanted to investigate what happens when too many lipids, fatty substances that make up different structures of the brain’s cells, are released from dying cells.
- Under normal conditions, lipids are broken down by cells of the immune system, known as phagocytes, keeping their levels under tight regulation.
- In comparison to other organs, the brain is particularly rich in lipids as many of the brain’s neurons are covered in a fatty layer, known as myelin.
- However, if lipid levels are too high, phagocytes become overwhelmed and build up too many lipids within small droplets, causing them to appear ‘foamy’.
- The scientists in this study hypothesised that build up of lipids and the formation of foam cells may make the inflammatory response worse and lead to the production of toxic molecules, which could contribute to cognitive decline in patients.
Aims of the study
- Firstly, they wanted to investigate what happens to the lipid levels in and around the area of brain injury after a stroke and whether this has any effect on the immune system.
- They also investigated whether a compound named 2-Hydroxypropyl-β-cyclodextrin (HPβCD), which prevents lipid build up inside phagocytes and stimulates an anti-inflammatory response, could be used as a treatment for cognitive decline in stroke.
What did the scientists do?
- The scientists induced a stroke in both young and aged male mice.
- A week after the stroke, some were given HPβCD 3 times weekly.
- The scientists compared the amount of different lipids and the levels of genes involved in inflammation and lipid breakdown between mice treated with HPβCD and those who were not.
- Finally, they used behavioural and memory tests to assess whether HPβCD had improved cognition.
What were the key findings?
- Mice who were not given HPβCD had much higher levels of lipids in the area of brain injury compared to the unaffected side of the brain. These lipids, which had come from the remains of damaged cells, were seen to be accumulating inside cells within droplets.
- These mice also had higher levels of genes involved in inflammation and lipid breakdown.
- However, mice treated with HPβCD had significantly less lipid droplets within cells and less immune cells were present in the area of brain injury, particularly B-lymphocytes, a type of immune cell thought to be important in cognitive decline.
- HPβCD also increased the level of genes involved in brain recovery and repair and restored the levels of genes involved in lipid metabolism.
- Lastly, mice treated with HPβCD performed better on cognitive tests and did not display any abnormal cognitive function, unlike untreated mice.
What next?
- To conclude, the results of this study have shown that build up of lipids can worsen cognitive decline after stroke. The compound, HPβCD, has shown positive results in improving lipid levels, reducing the chronic inflammatory response and bettering cognitive recovery after stroke.
- However, the results were performed in a single laboratory, using only male mice. Therefore, before this can be trialled as a potential treatment in stroke survivors, the same results need to be confirmed by other laboratories, using female mice also.






0 Comments